Adverse Events
Adverse events are events or errors that can cause unintentional harm to a patient as the result of medical intervention, rather than the underlying medical condition.
Most adverse events are preventable. Preventable events can result from poor communication, a lack of safeguards or checkpoints, or human error. Failure to follow recognized, evidence-based best practices or guidelines at the individual or system level can lead to an adverse event.
At Catholic Health, when an adverse event occurs, we fully investigate the occurrence and complete a root cause analysis (RCA) in order to determine the attributing factor(s). Findings may result in a change to a policy or procedure and/or education for our associates and providers.
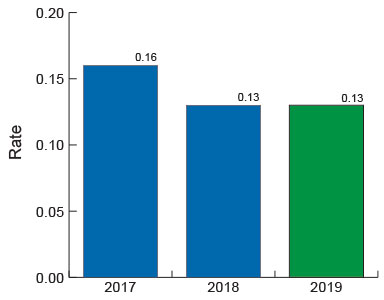
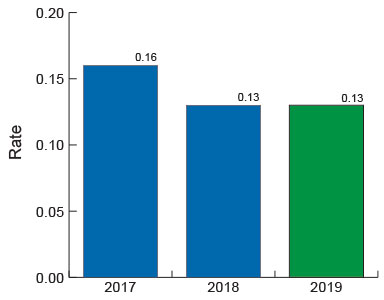
2019 Target: Less than 0.13 significant events per 1,000 patient days.
Back to top.